A Week of CBCT Imaging at Elm Endodontics in Broomfield, CO
Cone Beam Computed Tomography (CBCT) 3-D imaging is allowing us to more thoroughly evaluate, diagnose, and treatment plan root canal treatment at Elm Endodontics in Broomfield, CO. This post documents some of the unique cases seen during the week of June 28th – July 6th 2012, so that our readers can see that CBCT imaging adds value by allowing us to diagnose more thoroughly and approach treatment more specifically.
The following cases and their descriptions are not meant to be a comprehensive narrative on the presentation, diagnostic examination, treatment, or results. I have presented just enough information necessary to understand the benefit of cone beam imaging in the diagnosis and treatment of both “simple” and complex endodontic cases.
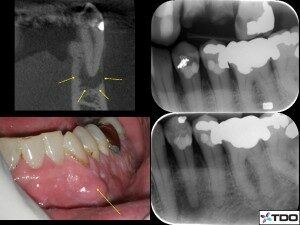
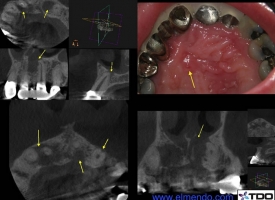
Case 1: Missed Lingual Canal on a Lower Incisor
This patient presented with failing endodontic treatment that was done greater than 10 years prior. CBCT imaging revealed uncleaned canal space on the lingual, uncleaned pulp horn due to an access positioned over the cingulum, and the presence of an apical radiographic finding consistent with apical periodontitis. Re-treatment endodontics confirmed the presence of an untreated lingual canal, that joined the buccal canal, and the presence of remnant pulpal tissue in the pulp horns (the clinician should remember that lower incisors have two canals 44% of the time). The canal spaces were cleaned and filled, and the access was restored with a light-cure composite. This is the third case like this in two weeks that I have treated.
I used information from the CBCT to better orient my access openings to get the best straight line access into the canal and to completely clean the pulp chamber without unnecessarily removing supportive tooth structure. This access is larger than I prefer on this tooth due to the previous access, which was too lingually oriented.
Also, some may suggest that the incomplete endodontic treatment on the adjacent tooth should also be treated. Since this tooth is asymptomatic and there is no evidence of disease, I preferred the conservative approach to monitor. (Click on thumbnails to see full images)Root Canal Retreatment CBCT
Case 2: Separated Instrument (Broken File)
This patient presented with a file that had been separated by his general dentist while attempting endodontic treatment. The file was positioned in the middle third of the DB root, and separated prior to thorough apical cleansing. CBCT imaging revealed the following:
- Presence of an apical finding on the palatal root consistent with apical periodontitis that has violated the sinus floor.
- Presence of localized sinus inflammatory disease likely related to the endodontic infection.
- A large MB canal and no MB2 canal.
- Presence of the file in the middle of the DB root
- No radiographic evidence of apical periodontitis on the MB or DB roots.
The file was removed without complication and the remaining canal systems were cleaned and completed. CBCT imaging was helpful mostly for gaining an understanding of the curvature of the DB root, the exact extent of the palatal root pathosis, and the absence of the MB2 canal. Since the MB2 canal was confirmed to be likely absent, the structural integrity of the tooth did not need to be compromised in its search.Separated Instrument Removal CBCT

Case 3: Abscess and Oral-Antral Sinus Tract
This patient presented on an emergency basis with swelling associated with an abscess on tooth #7, which was highly mobile. Previous endodontic treatment was present along with a post and crown. A palatal sinus tract was also present that produced purulence when the patient created positive pressure by plugging her nose while blowing. Tooth #10 was missing, and the patient reported that it was previously palatally impacted, orthodontically re-positioned, and later extracted. CBCT imaging revealed the following:
- Prior endodontic treatment, post, and crown on #7 with an incomplete apical obturation.
- The presence of a radiographic finding on #7 that wraps up the side of the root to the level of the post – a finding consistent with a possible root fracture.
- A large radiographic finding on the apex of tooth #11 that communicated with the floor of the nose.
- A buccal notching in the cervical area of #11 possibly consistent with resorption (ECIR).
CBCT imaging allowed for a much more thorough evaluation of the case that was not achievable with traditional periapical radiographs. The abscess was drained and the patient was placed on an antibiotic. Follow-up treatment will involve re-assessment of the abscess and mobility on #7 after one week. Root canal re-treatment will be initiated to treat the uncleaned canal space and to evaluate the possible presence of a root fracture. Treatment will also involve multi-visit endodontic treatment of tooth #11 until the sinus tract heals. The possibility of a neoplasm associated with tooth #11 cannot be entirely ruled out.Oral-Antral Sinus Tract

Case 4: ECIR of a Lower Pre-Molar
This patient presented still anesthetized from a crown preparation on tooth #28. During the process of preparing and radiographing tooth #28, the presence of a cervical radiolucency was noted on tooth #29. A buccal pocket of 6 mm with suppuration was present.
CBCT imaging revealed that a buccal radiographic finding consistent with ECIR (cervical resorption) was present that extended to the canal space. Prior endodontic treatment was done around 1995, and historical radiographs show that the resorption was not present as late as 2005, indicating that it began some time during the last seven years.
An unfavorable long-term prognosis was given with repair and possible root canal re-treatment if contamination of the canal was determined to be present. The treating dentist was contacted and consulted so the possibility of a bridge or implant could be discussed. The lab order for the crown on #28 was put on hold while the patient appoints to discuss options further with her dentist.
CBCT imaging allowed us to thoroughly diagnose the location and extent of the resorption, that otherwise could not be determined without surgically exposing the area in an attempt to treat the defect.ECIR CBCT

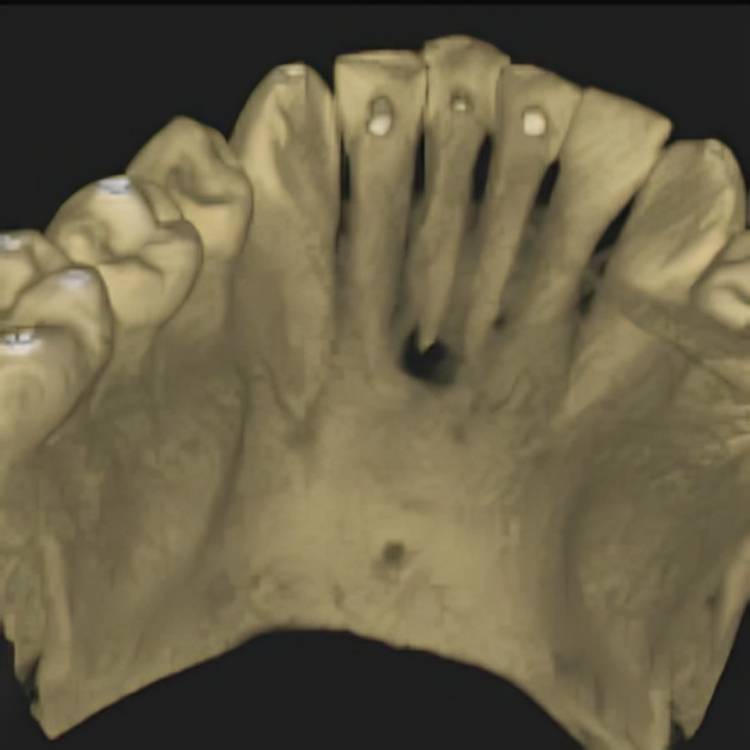
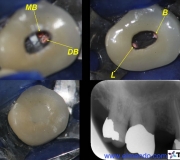
Case 5: Surprise! A Three Canaled First Premolar.
This patient presented with percussion sensitivity on tooth #5 associated with a necrotic pulp and apical periodontitis. Endodontic treatment was initiated without CBCT imaging since the case was expected to be fairly routine. When the canals could not be quickly located due to calcification a CBCT image was taken.
Axial slicing revealed the presence of a root structure suggestive of three canals. Over the course of three appointments the three canals were located and fully treated. The MB canal was the most difficult to find given that its orifice was located along the mesial wall of the DB canal. A fiber post was placed in the lingual canal for support, and the access restored with light-cure and dual-cure composite bonded to dentin and porcelain.
Had this case not been assisted by CBCT imaging, it would have been easy to be satisfied with treating the two canals, since three canals are present less than 10% of the time (some studies suggest that three canals are present less than 5% of the time).Three Canaled First Premolar


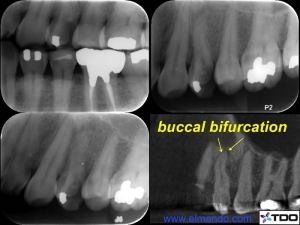
Case 6: First Premolar with Two Canals and Three Portals of Exit
This patient presented with percussion sensitivity on tooth #12. A crack was present along the mesial marginal ridge, and the tooth was in heavy occlusion. A CBCT image was taken to evaluate any defects in the bone that would suggest the presence of a root fracture. CBCT imaging revealed that the coronal bone structure was within normal limits, but careful reading of the volume revealed that an apical bifurcation of the buccal canal was present. The measuring tool revealed that the bifurcation occurs at the 16 mm mark, and that the remaining canal length is an additional 4 mm. The two main canals were cleaned at the first appointment. The bifurcated canal could only be located on one occasion with multiple attempts of searching with pre-bent files. The patient was re-appointed to continue treatment on another day.
CBCT imaging assisted in the discovery of a difficult to find canal that, if left untreated, may allow for persistent apical periodontitis and latent endodontic related failure. It is very likely that this canal would have gone untreated had CBCT imaging not been used.Apical Bifurcation
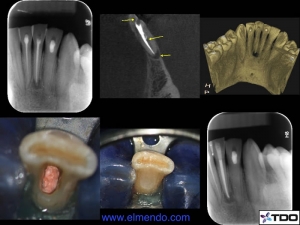
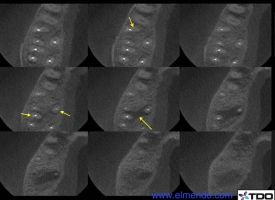
Case 7: Paired Apical Periodontitis
This patient presented with mild symptoms in the upper right. Prior endodontic treatment was done by a general dentist a few years prior. Periapical radiographs suggested the presence of apical pathosis, but the exact location was unclear. The radiographs suggested that the pathosis could be associated with the palatal root of #3, the DB root of #3, or the MB root of #2.
CBCT imaging revealed the presence of a radiographic finding consistent with apical periodontitis that extended from the palatal root of #3 to the MB root of #2 and was continuous. Missed (untreated) MB2 canals were present in both teeth.
Endodontic re-treatment was recommended for both teeth, and was initiated on tooth #2. Thermafill carriers were removed from three canals, the untreated MB2 canal was located and cleaned, and all canals were medicated with calcium hydroxide. The two teeth will likely be completed over the course of two more appointments.
Without the assistance of CBCT imaging, the true nature of the periapical pathosis could not have been ascertained. In a case where one lesion is shared by two teeth, both teeth may be contributing to the pathosis and need to be treated together or the infection may not heal.Paired Apical Periodontitis CBCT

Summary
Our readers should take away from this article that CBCT imaging is a great tool in making a thorough diagnosis in order to render complete and predictable treatment. In the past, when CBCT technology was not available, most of these cases would have left the clinician unsure of the exact etiologies and extent of disease, which would cast an ever-present shadow of doubt or failure over the course of treatment and recovery.
Another beauty of this technology is that radiation for these scans amounts to about that received from four periapical radiographs. In the past I would have had to take at least that many additional radiographs before, during, and after treatment to gather more information, but CBCT imaging allows me to gather more information with less radiation.
Bottom line is that both the patient and the clinician win. If your patients aren’t being seen in our practice, are they receiving the benefit they deserve and that modern technology can offer them?